Closing deals and having a loyal customer base are important, but what is equally crucial when it comes to the success of your business is how you manage your customer data.
And the key to proper data management is often an effective CRM tool, such as Salesforce.
Why?
Because it helps you connect all the important data, in one place.
Take surveys as an example. While they are one of the best ways to collect customer feedback, connecting that data with your CRM is when you truly take it to the next level. Synching the data from survey answers to CRM contact profiles or even triggering workflows based on survey answers.
Salesforce seems to be one of the most important tools for companies, it helps to connect everyone on the company, from leadership to CS or marketing teams with the right data. Therefore, the possibility to integrate it with a survey tool is equally essential when choosing the best option.
In this article, we'll analyze 10 best Salesforce survey tools to help you choose the best survey software for one of the most powerful CRMs out there.
We take into account the available features, pricing, the nature of the integration, and more.
Let's jump right in.
Salesforce is the CRM king
Salesforce is the world’s leading cloud-based Customer Relationship Management tool. In 2021, the company generated over $21 billion in revenue, with more than 166,000 websites worldwide using its solution.
It helps businesses level up and get ahead of the competition by getting to know their customers better every day. Salesforce combines customer feedback analysis, data management, and process automation.
What makes Salesforce attractive for sales reps particularly is its ability to integrate with other tools and systems, helping them create a cohesive ecosystem with all the important data.
Survey tools + Salesforce: what's the deal?
Survey tools are an integral part of the Salesforce toolbox, and it's not hard to see why.
They:
✅ let you collect data on sales activities more simply and efficiently,
✅ can give you a competitive advantage over other companies,
✅ provide access to large volumes of valuable customer data, which you can use to make informed decisions on products, marketing strategies, and customer service initiatives,
✅ automate the process of capturing data,
✅ make acting on data effortless with logic and workflows triggered based on survey data.
Now, the key thing is just choosing the software that integrates with Salesforce exactly how you need it to. 😉
Take a look at our list of 10 best Salesforce survey tools to help you choose the one.
#1 Survicate
Integrating sales and customer insights has never been easier since Salesforce and Survicate joined forces.
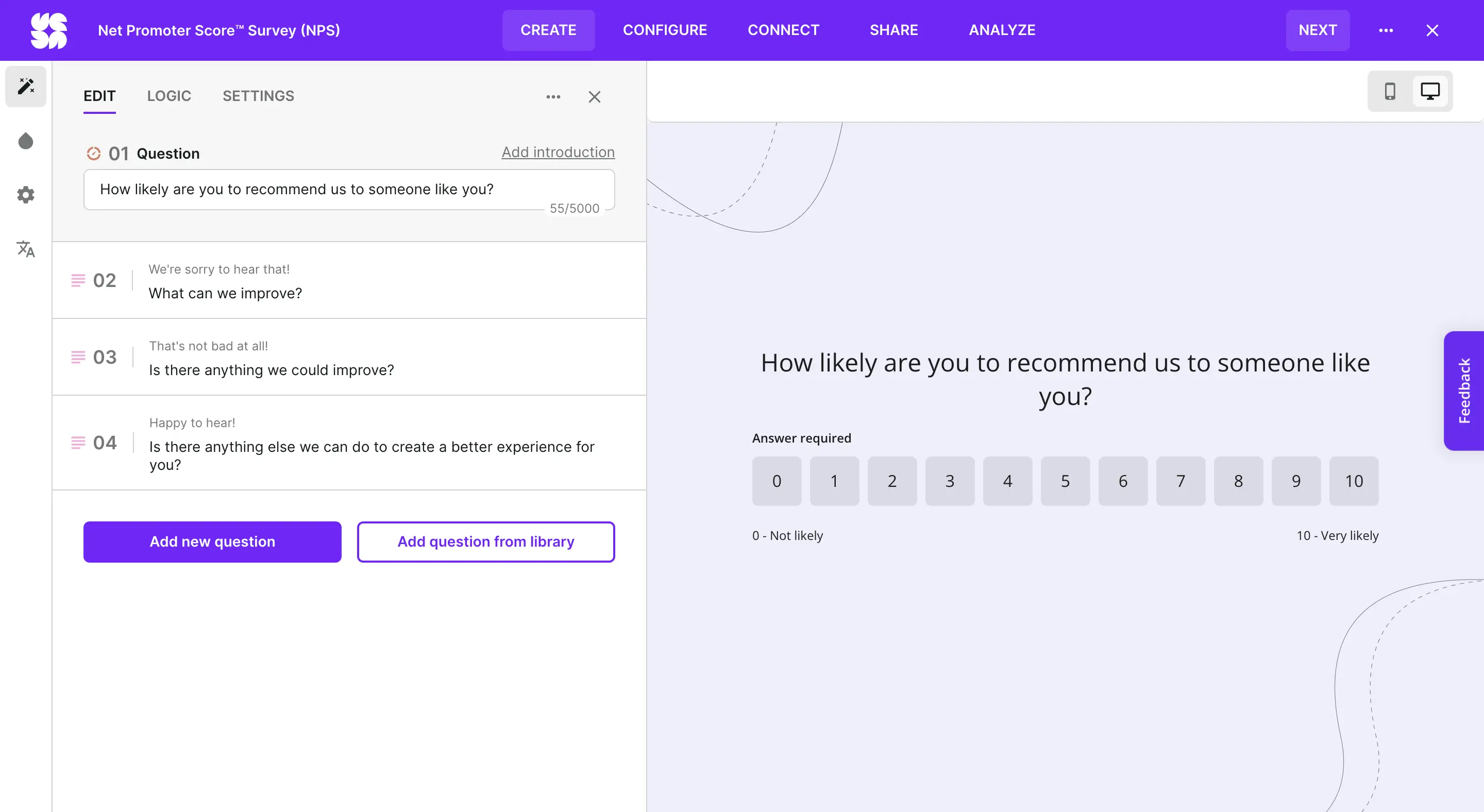
Survicate offers more than hundreds of professional survey templates that are responsive and tailored to different use cases. You can easily customize them to your liking, create surveys from scratch, use AI to build your surveys, and distribute them via email or link, embed them on your website or place them directly in your app.
While Salesforce gives businesses a powerful platform to manage sale opportunities, Survicate is the perfect solution for capturing real-time user feedback to inform business decisions.
Together, they provide an unbeatable combination, bringing full transparency to the customer journey.
Now, the integration between Survicate and Salesforce works both ways.
You can transfer data from your Survicate surveys into Salesforce and sync Salesforce data to Survicate. This makes it real easy to keep all your data working for you in harmony.
In a more down-to-earth explanation, this basically means embedding Survicate surveys into Salesforce emails, triggering workflows in Salesforce based on the received responses, automatically creating and updating contacts and leads in Salesforce, or syncing the Salesforce data with Survicate for AI analysis, filtering, and more.
The most popular use cases for using Survicate with Salesforce are tracking NPS and CSAT scores based on surveys run in Survicate to then:
- trigger notifications to different teams, for example, notify the Customer Success team about identified detractors,
- trigger emails in Salesforce, for example asking identified promoters for a review,
- create custom dashboards in Salesforce to monitor the CX metrics, giving you a bird's eye view of the important feedback data.
But that's not all.
You can also use both tools to level-up your feedback analysis game. For example, by creating dashboards with survey responses in Salesforce or by using one of the most unique features listed in this article—Insights Hub.
Survicate's Insights Hub is here to automatically analyze your feedback data, no matter its source, including—you guessed it—Salesforce.
You can pull the data from Salesforce and let Survicate's AI analyze it for you, automatically extracting insights and categorizing the data into topics.
%2520(1).webp)
We also have to heavily highlight the fact that Survicate offers a no-code, one-click integration with Salesforce, making it pretty easy to get started and connect both tools.
Last, but not least, users leaving reviews on G2 when asked about what they like about Survicate most list integrations as part of their answer. Like this user here saying: "Integrations - Marketo and Salesforce work great."
PS: if you want to dive deeper into this Salesforce survey tool integration, watch a dedicated webinar. It explains everything bit by bit.
Feature highlights
- One-click integration without coding
- Mapping survey responses to Salesforce objects, both standard and custom
- Sending surveys based on Salesforce segments and lists
- Triggering Salesforce workflows based on survey responses
- Triggering emails in Salesforce based on survey responses, for example asking for a G2 review
- Syncing Salesforce data with Survicate's Insights Hub for automatic AI analysis
- Building custom Salesforce dashboards with survey responses
- Identifying Salesforce contacts and leads
- Notifying team members based on NPS/CSAT scores, for example after identifying promoters
- Testing the integration in a sandbox environment
- Syncing Salesforce contact data with Survicate to filter data analysis and exports
Pricing
The Survicate and Salesforce integration is available on the Better Than The Rest plan, giving you a direct way to gain valuable insights into what makes your business tick.
This plan starts at $299 and comes with everything that Survicate has to offer, from all the survey types and distribution channels to AI survey analysis, to custom CSS design and a dedicated Customer Success Manager at your side.

#2 SurveyMonkey
SurveyMonkey is a survey software that helps build different types of surveys, from CSAT to NPS ones, and share them with clients using various methods. SurveyMonkey has been on the market since 1998, targeting a plethora of niches, from marketing to healthcare.
The integration of SurveyMonkey with Salesforce allows you to automate web, link, and email-based surveys to be sent based on Salesforce triggers, as well as sync data back into Salesforce for analysis and reporting.
Some of the most popular use cases listed by SurveyMonkey for this particular integration include measuring CSAT or NPS scores, sending feedback surveys to customers post events, sharing surveys after winning or losing sales opportunities, or creating new leads in Salesforce after identifying them with SurveyMonkey's lead capture forms.
Surveys can be sent using a web link or SurveyMonkey email invitations, both of which can be integrated with Salesforce flows. Web links allow for customized survey logic, while email invitations can be triggered directly from Salesforce actions (e.g., after closing a case.)
The integration also supports creating new records and updating existing records. To be more specific, it allows partial response sync and offers query mappings to locate and update specific Salesforce records.
You can choose from two mapping types: a managed package for automatic response mapping or custom object mapping for tailored data needs.
Users leaving reviews for SurveyMonkey on G2 seem to be enjoying the Salesforce integration, some even praising the ease of implementing this third-party tool. Like this user here: "Documentation on how to setup is easily laid out and you don't need to be a super technical person to be able to provision."
Feature highlights
- Triggering SurveyMonkey surveys to be sent via Salesforce using the Salesforce flows
- Creating and updating records using the different mapping options to Salesforce objects (like account, case, contact, etc.)
- Sharing the mapping fields you create with other team members,
- Copying mapping fields between sandbox and production environments.
Pricing
The Salesforce integration is in most cases an advanced tool connection, and it's no different in SurveyMonkey. This integration is available solely on the highest-tier plan, Enterprise, and as an add-on too.
Now, to know how much connecting both software may cost you, you need to get in touch with SurveyMonkey's sales team, but prepare for a rather costly solution.
#3 Zonka Feedback
Zonka Feedback is yet another survey software, or even more so a customer feedback platform, covering multiple channels and use cases. From regular CSAT or NPS surveys to in-product surveys or even offline kiosk ones.
Zonka Feedback integrates with Salesforce natively and makes it possible to sync survey responses and update Salesforce objects in real time.
Basically, we get two mapping options: custom mapping, where survey fields are manually mapped to Salesforce objects, and managed mapping, which automatically syncs customer data and CX metrics.
The integration allows users to create and update Salesforce objects, sync locations and response tags, and perform sentiment analysis. Additionally, users can configure syncing options based on Salesforce Contact IDs or email addresses and automatically create new contacts if a match isn't found.
Feature highlights
- Manually mapping fields to Salesforce objects for real-time data syncing based on received responses
- Automatically mapping fields for Salesforce contacts
- Syncing CX metrics and sentiment values
Pricing
Probably not a surprise at all, but the Salesforce integration is once again available from the Enterprise plan in Zonka Feedback, whose price is established on a custom basis. But you can purchase the Salesforce integration as an add-on if the Enterprise seems a bit over the top.
However, Zonka Feedback's help center shares different information, stating that custom mapping is available for every Zonka Feedback plan, while automatic mapping, aka the managed one, is available from the Growth plan.
In that case, it would be best to just get in touch with Zonka Feedback's sales or support team to confirm which pricing information regarding the Salesforce integration is true.
#4 SurveyLab
SurveyLab is a survey software that allows you to build and distribute your surveys in a myriad of ways, from SMS to QR codes and website widgets. Besides just working on your surveys, you can of course analyze the responses just as well, and integrate with third-party tools to take the survey feedback to the next level.
SurveyLab offers quite a few integrations, with Salesforce being one of the native tool connections.
Unfortunately, the integration doesn't go too far—only making it possible to embed SurveyLab surveys in emails sent out from Salesforces. Not much in comparison to other Salesforce survey tools listed in this article.
Feature highlights
- Embed SurveyLab surveys in Salesforce emails
Pricing
APIs and integrations are available on the Enterprise plan, but the Salesforce integration specifically, is available on both the Professional and Enterprise plans.
The Professional plan costs $249 monthly.
#5 Qualtrics
Qualtrics is an advanced research solution that offers flexibility and customization—but it might not be right for everyone. It targets enterprises and those with big feedback needs specifically.
The Salesforce integration in Qualtrics is pretty extensive, just like the whole software.
Some common use cases include sharing CSAT surveys for closed cases in Salesforce, collecting feedback based on recent purchases, or distributing surveys to an entire list of Salesforce contacts.
To be more specific.
You can automatically trigger a feedback survey when a case is closed and link the feedback to related objects like contact, account, and case.
Second, you can trigger surveys after account changes occur, such as purchases, renewals, or cancellations, and store responses in a custom object linked to the account.
Third, you can distribute surveys to entire Salesforce Campaigns or use third-party extensions for bulk distribution or guided interviews directly on contact records in Salesforce.
Feature highlights
- Creating new leads in Salesforce from your Qualtrics survey
- Using advanced logic to decide which respondents will be saved into Salesforce and which will not
- Triggering surveys to be sent in Salesforce emails
- Mapping data from your Qualtrics survey into Salesforce records and choosing to insert, update, or delete records for both standard and custom objects
- Downloading Qualtrics from the Salesforce AppExchange to access Qualtrics from within Salesforce
Pricing
Unfortunately, Qualtrics does not provide pricing information upfront. To learn how much Qualtrics and integrating it with Salesforce may cost you, it's best to reach out to Qualtrics team directly.

#6 Wufoo
Founded in 2006, Wufoo is yet another online form builder that helps you collect customer data, but also payments and files—making it more than just feedback collection software.
Wufoo integrates with many third-party tools, Salesforce being one of the available options.
But don't expect too much connecting Wufooo with Salesforce.
This is yet another integration that doesn't go too far—allowing us to basically create new contacts or leads in Salesforce based on form responses in Wufoo and view survey respones in Salesforces.
A little treat is the possibility to use custom logic to control which form fields sync with Salesforce—but that's about it for this one.
Feature highlights
- Collecting feedback with Wufoo and analyzing respones in Salesforce
- Creating new contacts or sales leads in Salesforce based on form responses in Wufoo
Pricing
What features don't make up for, the price in this case definitely does. All integrations, including the one with Salesforce, are available from the Starter plan in Wufoo, costing you just short of $15 a month.
#7 Simplesat
Based in Hong Kong, Simplesat is a customer feedback software that lets you collect and measure feedback data. It's mostly focused on email-based surveys, from sharing NPS, CSAT, and multiple-question surveys.
Simplesat of course integrates with Salesforce, just as other tools listed in this article, and this one is pretty extensive.
The integration lets you create custom feedback objects and update contact and case fields, providing more control over customer satisfaction data. It also works both ways, allowing you to sync data from Simplesat to Salesforce, and other way round.
You can map Simplesat feedback to Salesforce contacts, cases, and custom objects, including updating contact and case fields with metrics like CSAT, NPS, or sentiment. You can also sync contacts, cases, and account details from Simplesat to Salesforce, creating new entries if they don’t already exist.
Simplesat users make a note of the Salesforce integration, like Tannile B. did on G2 saying: "Simplesat makes working with our customers more manageable, and I love that it integrates seamlessly with Salesforce, Zendesk and Slack."
Feature highlights
- Real-time syncing of feedback details with Salesforce
- Generating reports within Salesforce
- Including surveys in existing Salesforce notifications
- Syncing case and contact data from Salesforce to Simplesat
- Displaying survey feedback in Salesforce internal comments
Pricing
The Salesforce integration in Simplesat is available from the Pro plan and up, which starts at $249 per month when billed on a monthly basis.
#8 ProProfs
ProProfs is a tool that offers many products, such as tools for creating knowledge bases, building live chats, working on courses and quizzes, and more. But it also offers a Survey Maker tool, which integrates with Salesforce.
ProProfs Survey Maker integrates with Salesforce to help you connect with your favorite CRM. It basically syncs the data you collect in ProProfs with Salesforce.
But we're listing it as #8 on the list since it's not nearly as extensive as other survey tools integrating with Salesforce, discussed above.
The whole tool connection comes down to syncing survey responses and triggering surveys to be sent from Salesforce. Now, the responses land directly into Salesforce to then create new leads or contacts or analyzing the feedback directly in your CRM.
In turn, triggering surveys to be sent works based on Salesforce events, such as an upcoming subscription renewal or your pricing changing.
Feature highlights
- Syncing data between ProProfs Survey Maker and Salesforce
- Analyzing survey responses directly within Salesforce
- Creating leads in Salesforce by mapping survey responses into fields
- Automatically triggering sending surveys based on Salesforce events
Pricing
The cost of using ProProfs Survey Maker differs based on the responses you anticipate to collect. For example, the free version of the software goes up to 50 responses a month, while the payable Business plan costs $79.99 monthly per each 100 responses you collect.
Salesforce integration specifically is available on both plans, even the free option, however, do keep in mind the heavy response limits.
#9 Surveypal
Surveypal understands that customer feedback can be a huge undertaking, so it aims to take the stress out—but it definitely focuses more on the data analysis part.

Now, to get to the meat and potatoes—Surveypal's Salesforce integration doesn't really fall far from other tools listed in this article.
It makes it possible to trigger Surveypal surveys to be sent after Salesforce events, like closing a deal or a support case. You can also connect the feedback data you gather in SurveyPal to specific accounts, contacts, or opportunities in Salesforce for even more detailed insights.
Other than that, anticipate the possibility to analyze Surveypal responses directly in Salesforce.
One unique feature is definitely the fact that we can trigger automatic notifications to our team members in Salesforce after responses start showing up from the surveys we've also triggered.
Feature highlights
- Triggering survey sending based on Salesforce events or milestones
- Syncing survey feedback data with Salesforce for deeper analysis and reporting
- Automatically notifying team members of new survey responses in Salesforce
Pricing
Surveypal offers two plans, and the Salesforce integration is available right from the first-tier subscription "Survey tool". However, even though the integration is available on the first-tier plan, it's still quite expensive starting at 299 EUR.
The caveat lies in responses. Surveypal doesn't state how many responses you're getting on the basic plan, so if you are sure to get big response numbers, it's best to reach out to Surveypal directly to help estimate the final price.
#10 Mopinion
Mopinion is a feedback survey software that focuses on three main channels, which are website, email, and applications, allowing you to collect customer insights from different areas. When it comes to extending its power—Mopinion integrates with many different tools, including Salesforce.

Connecting Mopinion with Salesforce comes down to two main use cases: either creating a new support or service case in Salesforce with contact details and feedback from Mopinion or creating a new lead in Salesforce with the details and feedback.
Now, when it comes to the technical difficulty level here, don't expect a one-click integration as for example Survicate offers.
Connecting Mopinion and Salesforce is a tad more difficult.
You have to create webhooks and API endpoints in Salesforce in order for the integration to work. Besides, you also have to get in touch with Mopinion's support team, sharing the endpoint information you've generated so that the connection can be complete.
Feature highlights
- Creating new support or service sases in Salesforce, filled with the contact and feedback details from Mopinion
- Automating creating new leads in Salesforce based on the collected feedback in Mopinion
Pricing
Not only is integrating Mopinion with Salesforce quite difficult, it's also expensive. And that's not even because the integration itself is pricey or has its place in the highest-tier plan (such information is actually hard to find, so we're not quite sure). But, Mopinion is expensive on its own.
Plans start at $329 monthly, with only Mopinion Website features being available. If you'd like to extend your subscription to email or app feedback features, you can expect to pay over a $1 000 monthly, with limitations still breathing down your neck.
Survicate—the ultimate Salesforce survey tool
Salesforce is a powerful tool but equipped with one of the survey tools we’ve described above, it takes your customer success to an entirely new level.
The software you choose depends on your needs and budget. Some tools integrate with Salesforce both ways, others not necessarily. Some offer a lot of features, others not really.
But if you expect a lot from a survey tool integrating with Salesforce, we highly recommend our own software—Survicate.
It integrates with Salesforce natively, in a one-click, no-code manner. It works both ways, giving you the option to sync data from Survicate to Salesforce and other way round.
With it, you can easily embed professional surveys into Salesforce emails, create and update contacts and leads, trigger Salesforce workflows based on response data, sync Salesforce data with Survicate for automatic AI analysis and categorization, and so much more.
Track your NPS and CSAT scores collected based on Survicate responses, and use that data to automatically trigger team notifications, and take action right when it's needed.
Sign up for a free trial of Survicate, and see if it works with Salesforce the way you imagine it.
This article was originally written by Kinga Edwards.














